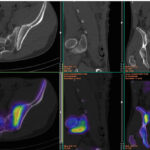
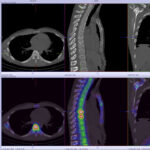
Back pain and Bone scans
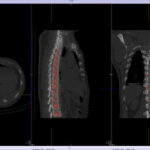
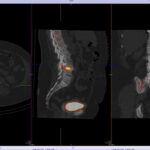
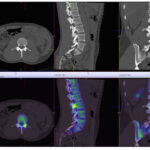
SPECT-CT bone scans of the spine have become a clinically useful part of the evaluation of back pain. Uptake seen on a SPECT-CT correlates with metabolic activity in bone and the increased resolution and specificity of SPECT-CT has allowed a greater number and variety of clinically relevant findings. Most patients with back pain will have an abnormality on high resolution SPECT-CT bone scan. Many of these will be clinically relevant and like all bone scans, it is sometimes the negative scan that is most helpful. The following diagnoses are best made or excluded using a bone scan:
The following diagnoses are best made or excluded using a bone scan:
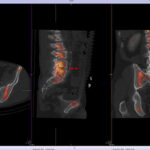
- Active facet joint arthropathy (as opposed to inactive disease which CT and to a lesser extent MRI show anatomic rather than functional changes)
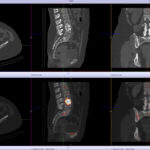
- Significant pars interarticularis fractures (MRI false negative 10%)
- Fractures
- Bridging osteophytes
- Stress fractures
- Vertebral fatigue fractures
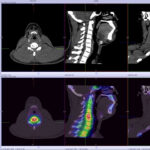
- Boney metastasis (though early lytic disease and lesions less than 5mm can be problematic for all imaging)
- In prostate carcinoma suggest bone scan if PSA>10, symptoms, Gleason score >7
- In breast carcinoma suggest bone scan in recurrent breast cancer or stage III,IV disease
- Post surgical fusion complications (>12months post surgery)
- Fusion failure -cold on scans done early post surgery (<8 months) and hot (>18months post surgery)
- pseudarthrosis
- adjacent segment disease
- screw impingement
- transitional vertebra with partial incorporation stress injuries (not seen generally on MRI)
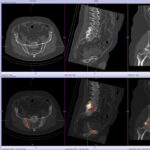
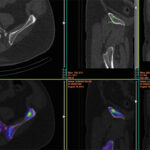
- Sacroliliitis
- Sacral, coccygeal and pelvic fractures
- Enthesitis at the adductor attachments, greater trochanters,
- Pseudarthrosis between joint variants (partially incorporated vertebra) or between posterior spinous processes
- heterotopic or dystrophic ossifications
In addition a bone scan is helpful in the investigation of back pain where other imaging is negative, does not correlate with the clinical findings, or has too many abnormalities. It casts a much wider net than either dedicated CT or MRI so has a role in defining poorly localised musculoskeletal pain.